Chronic kidney disease (CKD) is a condition characterized by a gradual loss of kidney function over time. The term chronic is used to refer to a condition which is permanent and irreversible. In addition, it progressively worsens even with treatment. This will eventually, over a period of time lead to need for dialysis or renal transplantation.
This is associated with complications such as high blood pressure, weak bones, low blood 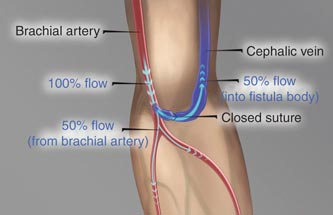
 hemoglobin and cardiac and nerve and brain damages.
hemoglobin and cardiac and nerve and brain damages.
Causes of Chronic Kidney Disease
The two main causes of chronic kidney disease are Diabetes mellitus and High blood pressure. These two diseases together are responsible for up to two-thirds of the cases.
High blood pressure, if uncontrolled, or poorly controlled, can be a leading cause of heart attacks, strokes and chronic kidney disease. Also, chronic kidney disease can cause high blood pressure.
Several other conditions can cause chronic kidney disease.
• Glomerulonephritis:A group of diseases that cause inflammation and damage to the kidney’s filtering units. These are unique diseases which generally affect the kidneys primarily and as a result of kidney damage can cause damage to other organs of the body. These disorders are the third most common type of kidney disease.
• Polycystic kidney disease An Inherited diseases, which causes large cysts to form in the kidneys and damage the surrounding tissue.
• Malformations and developmental abnormalities that occur during intrauterine development.
• Systemic lupus erythematosos and other diseases that affect the body’s immune system.
• Obstructions to urine flowcaused by problems like kidney stones, tumors or an enlarged prostate gland in men.
• Repeated urinary infections.
Most people may not have any symptoms until their kidney disease is advanced. However, the following symptoms occur as the disease progresses.
Tiredness and feeling less energetic in day to day activities; have trouble concentrating have a poor appetite and have difficulty in sleeping. These are non-specific symptoms and occur very slowly and are difficult to recognize in the beginning.
In addition patient may also have certain specific symptoms like swelling in the feet, and puffiness of the face especially around the eyes more so in the morning. Decrease in urination sometimes associated with the need to urinate more often at night occurs.
In severe cases and advanced renal failure patients have breathing difficulty, headache, convulsions, visual disturbances, and loss of consciousness. This warrants emergency treatment.
Detection of chronic kidney disease: Important tests of kidney function.
The earlier kidney disease is detected, the better the chance of slowing or stopping its progression.
Blood Urea Nitrogen: This is a chemical which accumulates in the body during day to day activities. It is normally excreted by the kidney and it accumulates in the blood in patients in whom the kidney function is reduced.
Serum Creatinine: this is also a waste material which accumulates in the body and if not cleared by the kidneys its blood levels raise. A raised blood urea and creatinine levels generally indicate kidney failure; however the values need to be interpreted taking in to account several other variables. Generally both blood urea and serum creatinine levels are to be considered.
If these tests are abnormal then several other chemicals in the body need to be measured to decide on the severity of the disease and to guide the treatment.
It is important to note that these tests indicate the severity of the disease and cannot confirm whether the disease is reversible or permanent.To decide if the damage is permanent or reversible renal scan is necessary
Ultra sound scan or CT scan of the kidneys will give information regarding the size of the kidneys and presence or absence of obstruction
In patients with Chronic kidney disease the kidney size is usually reduced to less than 9cms which is the normal size. In addition the appearance of the kidneys in the scan also is abnormal.
Kidney Biopsy:
In some patients if the kidney size is normal taking a small bit of kidney tissue though a needle and studying the microscopic structure may be necessary
Additional tests may be necessary to detect the complications or response to treatment measures.
Salient points:
Early detection can help prevent the progression of kidney disease to kidney failure.
Heart disease is the major cause of death for all people with Chronic kidney disease.
Hypertension can causechronic kidney disease and chronic kidney disease can cause hypertension
Persistent proteinuria (protein in the urine) means Chronic kidney disease is present and may in some cases lead to kidney failure.
High risk groups include those with diabetes, hypertension and family history of kidney failure.
Two simple tests can detect Chronic kidney disease: blood pressure, urine albumin and serum creatinine.
Treatment options
These include the following:
Supportive treatment in the early stages:
Renal replacement therapy when the disease is advanced:
Supportive treatment:
This is started when the patient has kidney failure but the degree of failure is not severe and the patient can be managed with medications and diet.
The aim of therapy is to
1. Control the symptoms
2. To delay the progression of kidney failure
3. To prepare the patient for eventual dialysis support.
Control of Symptoms:
These include medication to control blood pressure, blood sugars in patients with diabetes, and some medications to alleviate the problems due to alterations in electrolytes, water content of the body and the bone minerals. With strict control of blood pressure the progression of kidney failure can be significantly slowed down.
Diet:
Salt restriction:to control blood pressure and fluid accumulation in the body.
Fluid restriction: to control swelling and fluid accumulation
Low protein: Protein in the diet acts as an additional burden on the already malfunctioning kidneys. Moderate reduction in dietary protein intake is known to reduce the progression of the kidney failure.
Fruits; generally fruits are very rich in a mineral called potassium. This is normally excreted only through the kidneys. In conditions where kidneys are unable work normally potassium accumulates in the body. High blood potassium levels are harmful to the heart and require urgent treatment.
Dietary advice from an experienced dietician is very helpful.
Renal Replacement therapy:
There are two treatment options for kidney failure:
Dialysis (hemodialysis or peritoneal dialysis) and kidney transplantation
Briefly Dialysis means removing the waste products from the blood periodically with the help of an artificial kidney or the patient’s own abdominal membrane.
Transplantation involves placing a normal kidney surgically from a donor either living or cadaver.
Hemodialysis
Hemodialysis is a treatment that removes wastes and extra fluid from the blood.During hemodialysis, the blood is pumped through soft tubes to a dialysis machine where it goes through a special filter called a dialyzer (also called an artificial kidney). After the blood is filtered, it is returned to the bloodstream.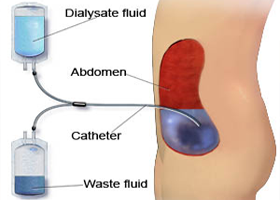
Dialysis is necessary if the kidneys no longer remove enough wastes and fluid from your blood to keep the body healthy. This usually happens when there is only 10 to 15 percent of kidney function left. The patient usually has severe symptoms such as nausea, vomiting, swelling and fatigue. However, one can still have a high level of wastes in the blood that may be toxic to the body and yet have minimal symptoms. Your doctor is the best person to tell you when you should start dialysis.
Blood is removed from the body using needles placed in the veins or through tubes inserted in to major veins. This is called dialysis access
(Images)
For the peripheral veins to give good amount of blood for cleaning a small surgery to connect the vein to the artery is required. This needs to be done several weeks before dialysis is anticipated.
Dialysis is generally required 3 times a week each time lasting for 4-5 hours. This can be done as an outpatient procedure and the patients usually can get back to work after the session is over. Blood tests are done monthly to assess the adequacy of dialysis.
Peritoneal dialysis:
In this process a small soft rubber tube is placed in the abdomen and once the wound heals sterile fluid can be instilled in to the abdominal cavity through this tube. The fluid is left in place for 3-4 hours and during this time it takes up the waste material from the blood and it can then be removed through the same tube. This is called one exchange. Usually 3-4 exchanges are required daily and the patient is trained to do the same at home. The quality of dialysis is assessed monthly by the Nephrologist.
Renal Transplantation:
This is the most physiological way of replacing the kidney function. It involves placing a new kidney in the patient’s body usually the lower abdomen. The kidney can be donated by a close relative or it can also be from a brain dead person. The donor and recipient pair undergo a series of tests to confirm mutual compatibility and matching. The recipient will require medications life long and close and frequent monitoring.
