What are bedsores?
A bedsore is an area of broken down skin and underlying tissue to form ulcers. Bedsores are also known as pressure sores, decubitus ulcers, pressure ulcers and pressure wounds.
What causes bedsores?
Bedsores are caused from a lack of blood flow and from mechanical stress to the skin and tissues over a bony area that has been under pressure for a prolonged period. If blood supply is cut off to an area of skin for more than 2 or 3 hours the skin is deprived of oxygen and begins to die. In addition, when slowly sliding down a bed or chair, friction to the outer skin layer such as from wrinkled bedding and clothing contribute to skin injury and ulcers. Excessive exposure to moisture such as sweat, blood, urine or faeces also increases the likelihood of bedsores.
Who is at risk of bedsores?
People whom are immobile due to illness or injury are at greatest risk of getting bedsores. These people may be wheelchair-bound or bedridden and are unable to change position without assistance. Also at risk are people whom, due to nerve damage from injury or illness such as diabetes or stroke, are unable to sense pain or signals that normally make people move. Elderly people are also at greater risk because their skin is thinner and more fragile.
Different pressure points on the human body while lying down
- Occiput or back of the head
- Both elbows
- Sacrum or lower back
- Both the gluteal regions or buttocks
- Both heels
What are the signs and symptoms of bedsores?
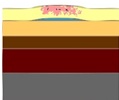
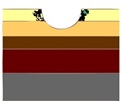
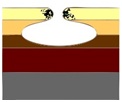
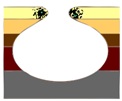
Bedsores are classified into stages according to wound severity.
What is the treatment for bedsores?
Bedsores can be difficult to treat once they go beyond stage 2. In the early stages when the skin is still intact bedsores usually heal by themselves once the pressure has been removed. Use of special ointments can prevent further bedsore infections. Once the skin is broken the main aim is to prevent infection and protect the sore so that it can heal. Special dressings may be used to help the healing process. Occasionally dead tissue may be removed with a scalpel (debridement, either in the ward or the patient may be required to be taken up in the operation room).
Therapeutic devices include:
- The newest and promising mode of therapy for pressure sore is Negative Pressure Wound Therapy NPWT) also known as Vacuum Assisted Closure (VAC).
- Hydrotherapy debridement, using saline solution in a syringe or water pressure jets.
- Chemical debridement using special debriding agent
Deep bedsores are very difficult to treat and often require surgical treatment to remove dead and decaying tissue. Sometimes healthy skin may be transplanted to the damaged area. Infections need treatment with antibiotics. In severe or life-threatening situations amputation of limbs may be necessary.
Can bedsores be prevented?
Bedsore can be managed if proper care is given to the bedridden patient from the very beginning.
- Correct malnutrition if present (fluid, energy, protein, vitamins and minerals)
- Daily inspection of an immobile person’s skin to detect early redness
- Frequent repositioning of the patient (recommendation is to turn them every 2 hours)
- Keep the skin clean
- Special foam, fibre and gels as padding materials used on chairs and beds to relieve the pressure on bony prominences
- Powered alternating-pressure mattresses and overlays
Prevention of bedsores is the best approach as established bedsores can be painful and life threatening. They also lengthen hospital stays and increase medical costs dramatically.